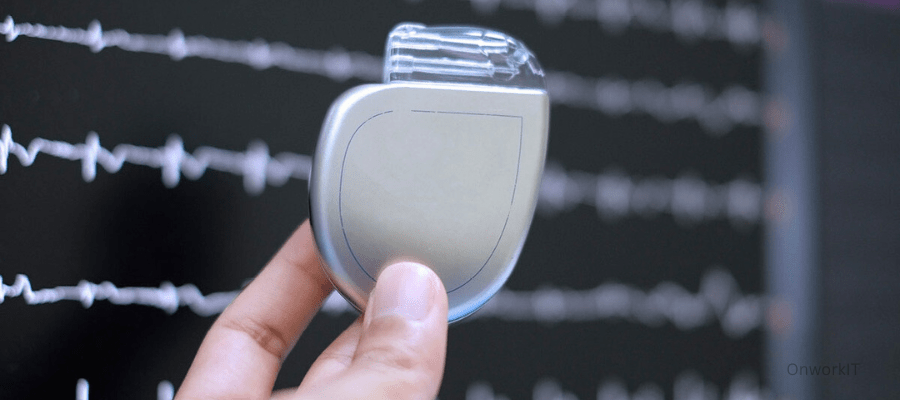
Understand “Artificial Heart” might sound like a magical machine capable of resurrecting the dead or transforming humans, but in reality, its official name ‘ventricular assist device’ reveals it has no such miraculous powers. Popularly known as an artificial heart, it’s simply a mechanical pump designed to help the heart ‘push’ blood throughout the body.
Who needs an artificial heart? It’s for patients with severe heart failure. As mentioned earlier, the heart’s main job is like a pump, constantly expanding (to let blood in) and contracting (to push blood out), ensuring a continuous circulation of blood throughout the body.
When the heart fails—when this pump can no longer function—the consequences are severe. Blood stops flowing through the body, oxygen and nutrients in the blood can’t reach where they’re needed, posing life-threatening risks. That’s when external help is necessary. The artificial heart is connected to the original heart via tubes, allowing blood to flow from the heart to the artificial one. The mechanical pump of the artificial heart then takes over, ‘pushing’ the blood back throughout the body. In simple terms, it’s using an artificial pump to replace the natural one.
What are artificial hearts used for?
As previously mentioned, when the heart loses its ability to ‘pump blood throughout the body,’ an artificial heart can step in to help. But the question arises: can an artificial heart permanently replace a natural heart, or is it just a temporary measure? To answer this, we need to understand under what conditions an artificial heart should be considered.

Reduces Risks
Firstly, it’s important to recognize that no matter how powerful an artificial heart is, it is still artificial and mechanical. The natural heart remains the best option for the body, as it reduces risks like organ rejection and abnormal blood clotting. Therefore, if a patient’s natural heart function shows signs of recovery, the artificial heart can be removed, allowing the natural heart to resume its job of ‘pumping blood throughout the body.’ In this case, the role of the artificial heart is temporary, serving as a ‘transitional therapy’ until the patient’s own heart can take over.
However, if a patient’s heart function is severely damaged with no chance of recovery, what can be done? The more definitive solution would be a heart transplant—replacing the damaged heart with a healthy, natural one, AI in healthcare.
Hold the Fort
Of course, heart transplants require donors, but as we know, donor hearts are scarce. This shortage is a global issue, with far fewer donors than patients in need of serious heart failure treatment. So, when a patient’s heart function is irrecoverable and a donor heart is unavailable, an artificial heart must be used temporarily to ‘hold the fort.’ Once a donor heart becomes available for transplantation, the artificial heart is removed.
In this scenario, the role of the artificial heart is similar to the first case—temporary assistance—but this time it’s for patients waiting for a heart transplant.
Another scenario where an artificial heart is necessary is related to heart transplants. If a patient’s heart function deteriorates rapidly—sometimes within hours—before the exact cause can be determined, the heart fails (‘the pump stops working’). In such emergencies, an artificial heart must be quickly deployed to save the patient. Subsequently, the patient’s natural heart function may recover, allowing the artificial heart to be removed. Alternatively, if recovery isn’t possible, a successful heart transplant becomes necessary, and the artificial heart supports until the transplant.
In this case, the role of the artificial heart is considered ‘transitional therapy’ while awaiting medical decisions.
Replacement Original heart into Artificial heart
The Final Scenario involves a new type of artificial heart. Recognizing the critical shortage of donor hearts and the unsuitability of some patients for major surgeries like transplants, scientists and doctors have improved artificial hearts. These advancements reduce complications, shrink the device’s size, and enhance durability. This ‘new type of artificial heart’ can be used long-term, potentially eliminating the need for a natural heart transplant altogether. Essentially, this ‘new type of artificial heart’ completely replaces the patient’s original heart.
In this situation, the artificial heart serves as the ‘end-stage treatment’ for patients with heart failure, meaning it’s the final treatment option without needing further changes.
Considering the various purposes and durations for which artificial hearts are used, as outlined in the four scenarios mentioned earlier, the duration of use varies. In the first three transitional therapies—’pre-recovery,’ ‘pre-transplant waiting,’ and ‘pre-medical decision waiting’—the artificial heart may be needed for just days to weeks. In contrast, for the ‘end-stage treatment,’ the artificial heart may need to function in the patient’s body for several years, even decades.
In Future Discussions
Given these differences in purpose and durability, it’s clear that there isn’t just one type of artificial heart. we will continue exploring the different types and brands of artificial hearts used worldwide, their distinctions, limitations, and their relevance to healthcare coverage.